Cruel Calculus: Reconciliation bill proves an intentional tool to deny healthcare access
Guest commentary by Nancy Heaton
Guest commentary by Nancy Heaton
The reconciliation bill signed into law on July 4th — paying for tax cuts by slashing healthcare access — represents a cruel and devastating blow to rural America. For the 17 towns where northwest Connecticut meets New York’s Greater Harlem Valley, these cuts aren’t abstract policy debates. They’re a direct threat to our neighbors’ survival.
In our 17-town region, the stakes are deeply personal. Based on statewide enrollment patterns, we estimate that roughly 32% of residents across our 52,000-person community — approximately 17,000 neighbors — depend on Medicaid coverage to stay healthy. This includes an estimated 8,000 children, representing about two-thirds of kids in our region. I’m talking about the cashiers at our local market, the home health aides caring for our elderly parents, the restaurant workers serving our families. What’s particularly striking is that 73% of the adults on Medicaid are working — they’re just caught in jobs that don’t offer decent health benefits.
When federal Medicaid funding — $6.6 billion annually in Connecticut and $62.4 billion in New York —gets cut, rural communities like ours face a perfect storm of healthcare collapse.
Rural healthcare operates on razor-thin margins. When Medicaid reimbursements drop, the domino effect is swift and merciless. Community health centers that serve regardless of ability to pay suddenly can’t meet payroll. Emergency departments become overwhelmed as uninsured residents seek primary care there, the most expensive setting possible.
For families scattered across our 17 towns, the nearest hospital might be 30 minutes away on a good day. When facilities close due to funding shortfalls, that distance becomes life-threatening. Transportation services currently provided by healthcare and social service organizations — often the only way elderly and disabled residents reach medical appointments — disappear overnight.
School-based health centers will likely be among the first casualties of healthcare cuts, and our communities will feel this loss acutely. Connecticut’s Region One School District and New York’s Webutuck Central School District have seen tremendous community support for bringing healthcare directly to students during school hours.
These programs aren’t luxuries, they’re necessities born from reality. When Foundation for Community Health began serving this region in 2003, we discovered that 60% of third graders had never received preventive dental care. Not because families didn’t care, but because the nearest dentists were hours away, requiring unpaid time off work that many couldn’t afford.
Over two decades, we’ve learned that preventive dental care correlates directly with overall health outcomes. Yet in February 2025, Community Health & Wellness indefinitely suspended dental services due to Connecticut’s inadequate Medicaid reimbursement rates. While other providers across the state may have quietly cut services too, ours was the only publicly announced suspension, a troubling sign that rural communities bear the brunt of funding shortfalls first and most visibly.
Healthcare cuts don’t just affect those who lose coverage, they devastate entire communities. When working families can’t access preventive care, we see sick children in classrooms, spreading illness and hampering learning. Healthcare costs will increase for everyone as emergency departments become primary care providers.
While Connecticut recently raised Medicaid reimbursement rates, the increase falls short of covering actual cost of care. Healthcare providers face rising wages, workforce shortages, and increasing procedure costs, while reimbursements remain inadequate. The math simply doesn’t work.
For rural providers serving large geographic areas with limited patient volumes, these financial pressures become existential threats. When the nearest alternative provider is hours away, losing even one clinic can leave thousands without access to care.
While the Medicaid cuts won’t take effect immediately, the reconciliation bill demands our urgent response now. The next two years present a window of opportunity to make our voices heard —and protect access to care — before these devastating reductions become reality. We still have the infrastructure and services that these cuts will eliminate, but only if we act.
This means reaching out to our representatives with the specific stories of healthcare access challenges in our region — the real experiences of families who drive long distances for routine care, or who delay treatment until conditions become emergencies. We need to share how working families in our 17 towns depend on Medicaid coverage, and amplify the voices of those already harmed by inadequate healthcare funding, like the families who lost access to dental care when Community Health & Wellness suspended services.
This is not the time to be quiet. Rural communities have always been resilient, but we cannot survive the deliberate dismantling of our healthcare infrastructure. Every resident of our 17-town region has a stake in this fight.
The overall health of our community depends on each of us demanding accessible healthcare for all.
Nancy Heaton is the President and CEO of Foundation for Community Health, serving northwest Connecticut and New York’s Greater Harlem Valley. She has over 30 years of experience in public health and has led FCH for 21 years.
There are artists who make objects, and then there are artists who alter the way we move through the world. Tim Prentice belonged to the latter. The kinetic sculptor, architect and longtime Cornwall resident died in November 2025 at age 95, leaving a legacy of what he called “toys for the wind,” work that did not simply occupy space but activated it, inviting viewers to slow down, look longer and feel more deeply the invisible forces that shape daily life.
Prentice received a master’s degree from the Yale School of Art and Architecture in 1960, where he studied with German-born American artist and educator Josef Albers, taking his course once as an undergraduate and again in graduate school.In “The Air Made Visible,” a 2024 short film by the Vision & Art Project produced by the American Macular Degeneration Fund, a nonprofit organization that documents artists working with vision loss, Prentice spoke of his admiration for Albers’ discipline and his ability to strip away everything but color. He recalled thinking, “If I could do that same thing with motion, I’d have a chance of finding a new form.”
What Prentice found through decades of exploration and play was a kind of formlessness in which what remains is not absence, but motion. To stand before one of his sculptures is to witness a quiet choreography where metal breathes, shadows shift and time softens.
After Yale, Prentice co-founded the architectural firm Prentice & Chan in 1965. The firm designed affordable housing projects in New York City, work largely led by partner Lo-Yi Chan. Prentice also designed custom single-family homes and continued to develop sculptural ideas alongside his architectural practice. After leaving the firm in 1975 and eventually relocating full time to Cornwall, he undertook a range of local architectural projects while increasingly devoting himself to sculpture.
Prentice began producing larger-scale sculptural commissions in the 1970s, during a period of national expansion in public art funding tied to new building projects. His first major commission came in 1976 from AT&T, helping launch a career that would bring his kinetic installations to corporate, institutional and public spaces across the United States and abroad. While his work follows in the lineage of Alexander Calder and George Rickey, critic Grace Glueck observed that its “gently assertive character is very much his own.”
In Cornwall, Prentice established a studio devoted to designing and fabricating kinetic sculpture, where he continued working for decades. He had many assistants over the years including local artists David Bean, Ellen Moon and Richard Griggs. David Colbert worked with Prentice for many years, assisting with fabrication, installation and project development and in 2012, Prentice established Prentice Colbert Inc., helping ensure that fabrication and development of large-scale commissions could continue beyond his lifetime.
Colbert said Prentice could be imperious, but came to understand that he valued thoughtful critique over agreement. “That evolved into a free and easy give-and-take, along with some fierce arguments,” he said. “Our relationship was always developing, right through to the end.”
In the mid-1990s, Prentice was diagnosed with macular degeneration, a condition that gradually narrowed his field of vision. Rather than turning away from the visual world, he leaned further into it, focusing on movement, light and peripheral perception — on what could be felt as much as seen. The Vision & Art Project film documents this period of his life and the ways he adapted his creative process.
Even in his final years, Prentice continued experimenting. In the summer of 2025, he created a series of drawings titled “Memory Trees,” produced from recollection as his eyesight declined. The series sold out at the Rose Algrant show that August, offering a poignant example of an artist adapting and creating throughout their lifetime.
“He was interested in whimsy,” said Nora Prentice of her dad. “But he also worked seven days a week,” she said. “He’d come in for dinner and then go right back out.” His studio was known for its atmosphere of curiosity and play, with music often drifting through the workspace as sculptures moved overhead in careful, measured rhythms. His work reminds viewers how profoundly small movements shape perception, and how change itself may be the only constant.
In his poem “Among School Children,” William Butler Yeats asks, “How can we know the dancer from the dance?” Prentice offered his own answer. “I’m not making the dance,” he said. “The wind is making the dance.”
As Nora reflected, “I think that’s how he would want to be remembered: for making the wind visible.”
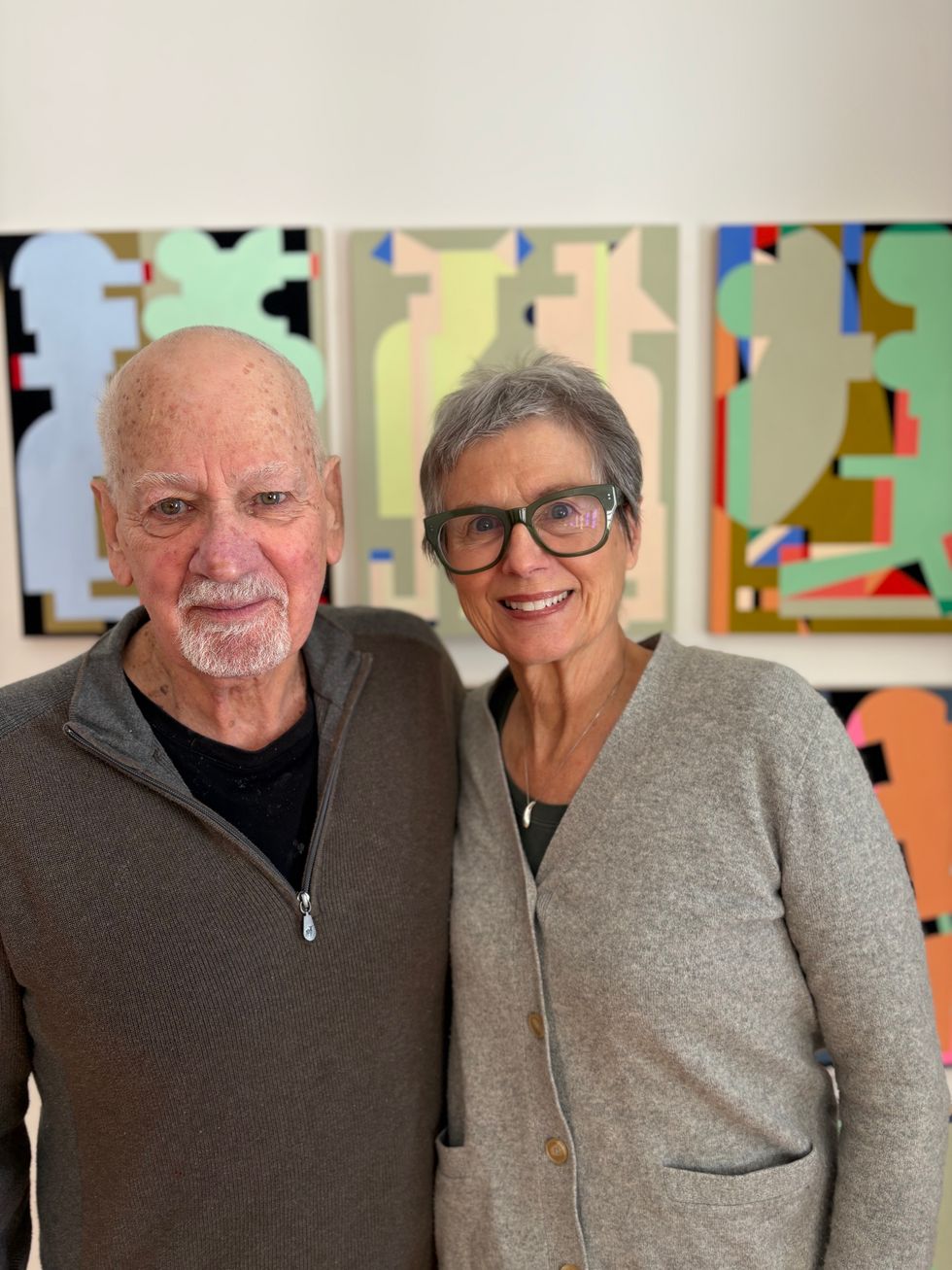
Laurie Fendrich and Peter Plagens at home in front of one of Plagens’s paintings.
He taught me jazz, I taught him Mozart.
Laurie Fendrich
For more than four decades, artists Laurie Fendrich and Peter Plagens have built a life together sustained by a shared devotion to painting, writing, teaching, looking, and endless talking about art, about culture, about the world. Their story began in a critique room.
“I came to the Art Institute of Chicago as a visiting instructor doing critiques when Laurie was an MFA candidate,” Plagens recalled.
“He was doing critiques with everyone,” Fendrich said of Plagens. “We met at one of those sessions and, well, what can I say. We fell in love instantly.”
Fendrich speaks candidly about the pressures that shaped her early life choices. “We both married the first time at 21, which a good number of women of my generation did without much thought.” Her first husband was a good guy, she says, but “we weren’t suited for each other at all, even though he suited my parents perfectly.” Her decision to get a divorce was seismic. “My mother didn’t speak to me for a year.” Time softened the rupture. “One day she told me, ‘I see now why you left.’”
Fendrich had a rigorous liberal arts education at Mount Holyoke. “I studied painting and drawing, but I also got interested in political philosophy. Plato, Aristotle, Machiavelli — Rousseau was my big guy — Tocqueville, everybody. And I still read them.” Plagens’s path was less formal. “I went to USC at 17,” he said, “and declared English as my major. It was a frat school, and I was in one for the first two years. Then I started doing the cartoons for the Daily Trojan, took a couple art classes, and thought, ‘Wait a minute, I like this.’”
Culturally, they diverged just as sharply. “I came from a fairly puritanical family that didn’t even go to the movies,” Fendrich said. Plagens, by contrast, grew up immersed in pop culture. “My father was an omnivorous reader,” he said, “and a jazz fan, and he shared these passions with me.” In 1966, Plagens walked into Artforum’s LA office and said, “I want to write reviews.” He was paid five dollars per piece. “Gasoline was 23 cents a gallon, so it went a long way.”
Over time, the couple slowly fused their educations. “He taught me jazz, I taught him Mozart,” Fendrich said with a laugh. “I’ve had a movie education from him; he read Jane Austen because of me.”
During their early years in LA, Plagens taught at USC, and Fendrich at Art Center College of Design. In 1985, they decided “our kind of abstraction would do better in New York,” as Fendrich put it. “So, we up and moved to Tribeca with $10,000 and a toddler.”
Both artists grounded their artistic careers in teaching and writing. “Teaching, which I loved, gave me the financial stability to be an artist,” Fendrich said, reflecting on her 27 years as a professor at Hofstra. “It meant that being an artist didn’t require I make money from every show. I didn’t start writing until 1999, but though I write for publication frequently, I make hardly any money at it.”
Artistically, they guard each other’s independence. “We have unspoken rules,” Plagens said. “You don’t comment on someone’s work while they’re in the middle of creating it.” Critique comes by invitation only. “He’s not mean, just direct,” said Fendrich. Over time, their aesthetics have subtly converged. “My work has gotten cleaner from looking at his,” she said. “He’s gotten more colorful because of me.”
The two have had several two-person exhibitions. At a recent duo show at the Texas Gallery in Houston “Laurie’s paintings flew off the wall,” Plagens recalled. “Me, well, not so much.”
Plagens’s parallel career in journalism shaped their lives in tangible ways. He worked as art critic at Newsweek from 1989 until 2003 and currently contributes reviews of museum exhibitions to The Wall Street Journal. “Being at Newsweek was one of the luckiest breaks I ever had,” he said. “They paid me to see things I would gladly pay to see.”
Their creative processes mirror their personalities. “I start with a specific idea,” Fendrich said, “and then modify things as I paint.” Plagens laughed. “I start with complete mush, just blurting it out and spending the rest of the time fixing it.”
In 2019, they made what Fendrich calls “a decision of contraction.” They left the TriBeCa loft they had lived in for three decades, sold their Catskills home with its large studio, and moved full-time to a former auto repair shop in Lakeville, now a house where each has a studio, and the ground floor retains the open feel of a loft.
What sustains them in life, art and love, decades in, are endless conversations — and arguments — about art, history, exhibitions, books and movies. That exchange, ongoing and rigorous, may just be the masterpiece of their shared life.
Hyalite Builders is leading the structural rehabilitation of The Stissing Center in Pine Plains.
For homeowners overwhelmed by juggling designers, architects and contractors, a new Salisbury-based collaboration is offering a one-team approach from concept to construction. Casa Marcelo Interior Design Studio, based in Salisbury, has joined forces with Charles Matz Architect, led by Charles Matz, AIA RIBA, and Hyalite Builders, led by Matt Soleau. The alliance introduces an integrated design-build model that aims to streamline the sometimes-fragmented process of home renovation and new construction.
“The whole thing is based on integrated services,” said Marcelo, founder of Casa Marcelo. “Normally when clients come to us, they are coming to us for design. But there’s also some architecture and construction that needs to happen eventually. So, I thought, why don’t we just partner with people that we know we can work well with together?”
Traditionally, homeowners hire designers, architects and contractors separately, a process that can lead to miscommunication, budget overruns and design revisions once construction begins. The new partnership seeks to address those challenges by creating a unified team that collaborates from the earliest planning stages through project completion.
“We can explore possibilities,” Marcelo said. “Let’s say the client is not sure which direction they want to go. They can nip that in the bud early on — instead of having three separate meetings with three separate people, you’re having one collaborative meeting.”
The partnership also reflects an expanded view of design, moving beyond surface aesthetics to include structural, environmental and performance considerations. Marcelo said her earlier work in New York City shaped that perspective.
“I had a 10-year career in New York City designing townhouses and penthouses, thinking about everything holistically,” she said. “When I got here and started my own business, I felt like I was being pigeonholed into only the decorative part of design. With the weight of an architect on our team now, it has really helped us close those deals with full home renovations, ground up builds and additions.”
The team emphasizes what it describes as high-performance design, incorporating modern building science, energy efficiency and improved air quality alongside aesthetic goals.
“If you’re still living inside 40-year-old technology and building techniques, we haven’t really handed off the best product we could,” said Soleau. “The goal is to not only to reach that level of aesthetic design but to improve the envelope, improve the living environment within a home and bring homes up to elevated standards of high-performance building.”
This integrated approach has proven particularly useful for renovation projects, where modern materials and systems can be thoughtfully incorporated into older structures. The firms also prioritize durability and long-term functionality, often incorporating antiques, vintage elements and high-quality materials designed to support clients’ lifestyles.
“I’m very big on investing in pieces that are going to be quality and last you the test of time,” Marcelo said. “Not just designing for a five- to 10-year run, but really designing for the long haul.”
The collaboration is already underway on several projects, including a major renovation in Sharon that involves rebuilding a 1990s modular home to maximize views while upgrading structural and performance systems. The firms are also exploring advanced visualization technology that would allow clients to experience projects through virtual reality before construction begins.
“For me, as somebody who wants to take the project all the way from beginning to end and make the process as effortless as possible for my client, it’s easier to do that with collaboration and a team than to do it alone,” Soleau said. “Most clients, especially second-home owners, want a team that can lead the project from concept through completion; aligning design, budget, and construction.”
On Feb. 19, the three firms will officially launch the initiative at an invitation-only event at The Stissing Center in Pine Plains, where Hyalite Builders is leading the structural rehabilitation of the historic building. A limited number of “hard hat tour” reservations will be available by request, providing rare, behind-the-scenes access while work is actively underway. Those interested in attending may contact event organizer Lauren Fritscher of Berkshire Muse at hello@berkshiremuse.com.