Latest News
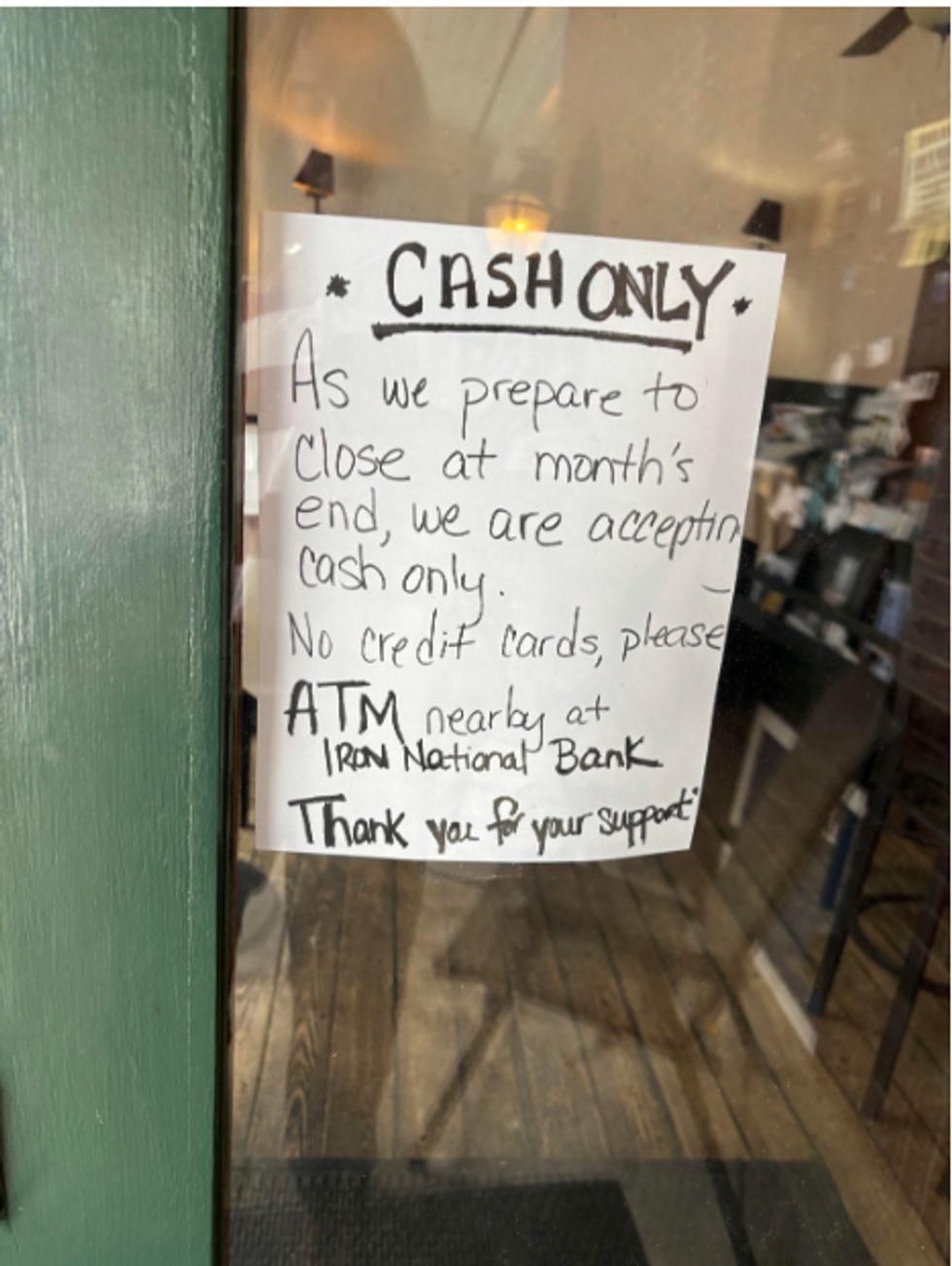
The Norfolk Pub, the town’s only restaurant and bar, will close at the end of the month, prompting concern among residents about the future of the Royal Arcanum building.
By Alec Linden
NORFOLK — The Norfolk Pub, the town’s only restaurant and bar, will close at the end of the month after 17 years in business, as uncertainty continues to surround the future of the Royal Arcanum, the hulking downtown building that housed the longtime institution.
On Wednesday, Jan. 7, the restaurant posted a notice on its doorway advising patrons that only cash will be accepted as “we prepare to close at month’s end.” The news has renewed speculation about what’s next for the Royal Arcanum, a Norfolk landmark that sold Sept. 8, 2025, for $1.4 million to American Folk & Heritage LLC, an entity associated with the prominent New York fashion brand Bode.
The Royal Arcanum, a large Arts and Crafts-style brick building, was built in 1904 by architect Alfredo Taylor as a home for the Norfolk Fire Department and several other town groups. Today, it houses the bookstore Les Renards & Co.; audiovisual consulting firm Boyce Nemec Designs, which has occupied a ground-floor office since the 1970s; Ruthann Olsson Interior Arts and Design; and the Pub. One of the commercial tenants, who requested anonymity, said their lease runs through Dec. 31, 2026.
The building also has contained additional office space and several residential apartments. According to a source close to the building, none of the residences were occupied at the time of the sale in September.
Local nonprofit the Norfolk Hub, which executed the sale, originally acquired the building in 2021 for $950,000 with assistance from a gift from the William and Mary Greve Foundation. In an Oct. 4 release, the group announced that $300,000 of the September sale proceeds had been allocated to the Foundation for Norfolk Living, a local affordable housing nonprofit, to support future housing projects.
An additional $500,000 was directed toward supporting the proposed firehouse project, according to the release.
The building’s new ownership — comprised of clothing designer Emily Adams Bode Aujla, her husband Aaron Aujla, an interior designer, and his brother Dev Aujla, CEO of Bode — has yet to announce plans for the Royal Arcanum, leaving many in town to speculate about what will occupy the vast structure.
Residents have been particularly concerned about the loss of the village’s only restaurant and bar, which has operated in the same location for decades under various names and owners.
Larry Hannafin and Sally Carr, both lifelong Norfolk residents with generations of family history in town, organized a petition in late December protesting the closure. “The pub is far more than a business,” the petition reads. “It is a vital gathering place, an economic anchor, a significant employer and a cornerstone of our town’s character.”
During an interview in late December with The Lakeville Journal, Hannafin and Carr expressed dismay at what they described as the loss of critical community infrastructure. “To live in a town that you can’t take a friend to supper with!” Carr exclaimed with exasperation.
“When I grew up there were five restaurants and five grocery stores,” Carr added.
Hannafin said he sent the signed petitions — which he last counted at 295 — to American Folk & Heritage on Wednesday. As of Friday, he said he had not received a response.
Dev Aujla said in a late December email to The Lakeville Journal that the closure followed a “conversation” between the new ownership and Norfolk Pub owner Heidi Forler. He did not elaborate and has not responded to follow-up requests for clarification. Forler declined to comment.
Norfolk Public Information Officer Jon Barbagallo said in late December that the town fire marshal was not involved, responding to circulating rumors that suggested otherwise. “This is strictly between the owners of the new building and the proprietors of the restaurant.”
Despite the imminent closure, the bar is maintaining its lively programming, with its popular trivia night returning on Wednesday, Jan. 14, followed by live music the following night.
Still, residents have begun mourning the loss of the town’s only watering hole and evening eatery, while looking anxiously toward the future.
A regular patron sitting at the bar Thursday evening praised the restaurant’s communal atmosphere. “Everyone knows everyone – it’s so great.” She described the closure as “tragic.”
First Selectman Henry Tirrell said Friday that the establishment has been a fixture his entire life and that he even spent the evening of his wedding day there. “It’s a sad thing to see it going away,” he said. “I certainly hope something can be restored there.”
Meanwhile, Lindsey Prevuznak, who has worked as a bartender at the Pub for a decade, announced the closure in a Facebook post Wednesday. Speaking with The Lakeville Journal on Friday, she reflected on the deep ties the establishment has with the community, describing its loss as “a heart break for entire community whose lives we enriched and touched.”
“I’m deeply grateful and humbled to have shared moments with such remarkable people.”
Keep ReadingShow less
Bryan Monge Orellana and Janneth Maribel Panjon Guallpa of Amenia are the parents of Ethan Nicolas Monge Panjon, Sharon Hospital’s first baby of 2026.
Photo provided
SHARON — Sharon Hospital welcomed its first births of the year on Wednesday, Jan. 7.
At 12:53 a.m., Ethan Nicolas Monge Panjon was born to Janneth Maribel Panjon Guallpa and Bryan Monge Orellana of Amenia. He weighed 5 pounds, 10 ounces and measured 20.25 inches long.
Later that morning, twins were born to Belinde and Erick Garcia of New Milford. Gabriella Garcia arrived at 8:17 a.m., weighing 5 pounds, 14 ounces and measuring 19 inches. One minute later, at 8:18 a.m., Isabella Garcia was born weighing 5 pounds, 8 ounces and measuring 18.5 inches.

Keep ReadingShow less
Area ambulance squad members and several first selectmen attend a Jan. 5 meeting hosted by Nuvance/Northwell to discuss emergency service providers.
By Ruth Epstein
FALLS VILLAGE — Paramedic coverage in the Northwest Corner is continuing despite concerns raised last month after Sharon Hospital announced it would not renew its long-standing sponsorship agreement with Northern Dutchess Paramedic.
Northern Dutchess Paramedic (NDP), which has provided advanced life support services in the region for decades, is still responding to calls and will now operate alongside a hospital-based paramedic service being developed by Sharon Hospital, officials said at a public meeting Monday, Jan. 5, at the Falls Village Emergency Services Center.
“We haven’t missed a beat; we’re still taking calls,” said Andrea Downs, president of the Falls Village Volunteer Fire Department and an employee of NDP, speaking at the meeting, which was attended by ambulance squad members, first selectmen and representatives of Sharon Hospital.
Sharon Hospital announced Dec. 11 that it would not renew its annual agreement with NDP, ending a 28-year relationship and initially stating that service would cease Jan. 1. Hospital President and CEO Christina McCulloch said the decision was based on compliance concerns tied to the hospital’s role as sponsor.
“Being a sponsor is a big deal,” McCulloch said. “Our concerns were big enough that we couldn’t sign. It was a difficult decision.”
She said the hospital had discussed the issues with NDP representatives and cited unmet state requirements.
Without a sponsoring hospital, NDP could not operate in Connecticut. That issue was resolved when NDP finalized an agreement with Stamford Hospital, allowing it to continue providing services in the Northwest Corner.
At the same time, Sharon Hospital is establishing a hospital-based paramedic service through Nuvance/Northwell, owner of the hospital. Under the current model, the service consists of a single paramedic, who begins the day at New Milford Hospital before traveling to Sharon, prompting concerns from some volunteer ambulance crews about response times while that paramedic is in transit.
Addressing those concerns, hospital officials said while the new paramedic service covers a wide area, so too does NDP, which is based out of Rhinebeck. Some volunteer ambulance crews also said their concerns relate to the transition to two providers, with Sharon Hospital’s service still being built out and not yet fully stationed in Sharon.
Falls Village First Selectman David Barger asked whether more than one paramedic service could operate in the region.
“There could be more than one,” McCulloch said.
Matt Cassavechia, director of emergency services for Sharon Hospital, said Litchfield County Dispatch, which handles all ambulance and fire dispatching for the region, will call whichever paramedic service is available at the time of an emergency.
He acknowledged that the current arrangement could be improved and said the hospital hopes to expand on-site paramedic coverage in Sharon. Doing so would require state approval through a need-for-service application, which Cassavechia said would benefit from letters of support from the community and area first selectmen.
Several volunteer ambulance representatives expressed concern about how changes could affect basic life support services and volunteer operations. Cassavechia said the hospital does not intend to replace volunteer squads.
“We’re not snapping up patients,” he said. “That’s not what we do. We are deliberate and purposeful. We have zero intent of putting volunteers out of business.”
Questions were also raised about possible delays in transferring patients from Sharon Hospital to other facilities. McCulloch said the hospital has been experiencing high emergency room and inpatient volumes but has not seen unusual wait times.
Michelle Hansen of the Falls Village ambulance squad cited a recent case involving a cancer patient who needed to be transported to Yale New Haven Hospital and was reportedly told by Nuvance that there would be an upfront cost of $2,000. NDP ultimately completed the transport.
“That is certainly not our practice,” said Thomas Horkan, Sharon Hospital’s EMS coordinator. “As soon as we were made aware, we took corrective action. It was human error. I listened to the tape. It was unfortunate.”
State Rep. Maria Horn, D-64, attended the meeting to assess how the changes might affect patient care and costs. Cassavechia said billing practices vary among ambulance providers and that clearer rules of engagement would need to be established with local squads.
After the discussion, Sharon First Selectman Casey Flanagan said the outcome appeared reassuring.
“It seems we’re going to have bonus coverage,” he said. “So, I’m OK with this.”

Keep ReadingShow less
Austin Howard Barney
Jan 07, 2026
SHARON — Austin Howard Barney — known simply as “Barney” to many, of Sharon, age 87, died on Dec. 23, after his heroic battle with the black breath, hanahaki disease, cooties, simian flu and feline leukemia finally came to an end.
Austin was born on July 26, 1938, son of Sylvester and Iva Barney.
He leaves behind an overwhelming amount of junk—sorry, treasures. If you’ve ever dreamed of owning a console TV roughly the size of a Buick, a soot-encrusted coffee pot that hasn’t been properly cleaned since the Reagan administration or creatively bent hangers that he had hanging in his living room windows to dry clothes on, give us a call. Please wait for the appropriate, respectful amount of time. Tomorrow should be fine.
Austin was frugal to the extreme; some may have called him “cheap,” but he preferred to think of himself as a pioneer in recycling—decades before it was cool. His kitchen was home to a vast collection of cool whip and country crock containers. The biggest challenge was finding actual cool whip or butter in his refrigerator with all the containers of leftovers that looked the same. “Open at your own risk” was our motto.
He leaves behind a wonderfully dysfunctional family—a group he tolerated, loved and occasionally avoided.
Austin was world-renowned for his lack of patience, grossly excessive extreme sarcasm, not holding back his opinion and knack for telling you exactly how wrong you were. One of his favorite quotes was, “I was only wrong once in my life. I thought I made a mistake.”
He always preferred his own cooking to anyone else’s—and to be fair, it was actually pretty good.
Austin served proudly with the 6th Marines in the United States Marine Corps from Feb. 10, 1958, through Feb. 9, 1962. Semper Fi!
He was also a volunteer fireman for several years, until he realized that sprinting in the opposite direction from fire was more aligned with his personal survival goals.
A natural mountain man, he ate things from the swamp that most people avoid and cooked on a wood stove for many years. He was an avid bird watcher and found joy in feeding all the animals that frequented his property.
He was predeceased by his brothers, Sylvester Barney, Louis Barney and his sister Shirley MacDougall.
He is survived by his daughters Darlene Hardzog, Margaret Gdovin (Mike); his son, Austin Barney Jr. (Kate); his grandchildren, Savannah Hardzog, Jordan Gdovin, Violet Barney, Amethyst Barney and Austin Barney III; and his sister Anita Baird along with various other relatives. You know who you are. He will be greatly missed.
There will be no viewing, as his children refused to comply with his request to be taxidermied and propped in the corner with a beer or a glass of scotch in his hand so guests could admire him in his natural state.
Services are pending and details will be shared at a later date.
In lieu of flowers, donations may be made to the American Red Cross in his memory.
Austin Barney has approved this message. Approval notwithstanding, it would have read the same.
Keep ReadingShow less
loading